Lung Cancer Part-1
Lung Cancer Symptoms and Signs
Lung cancer is the most common cancer in men and the fifth most
common in women, even causing more cancer-related deaths in women than
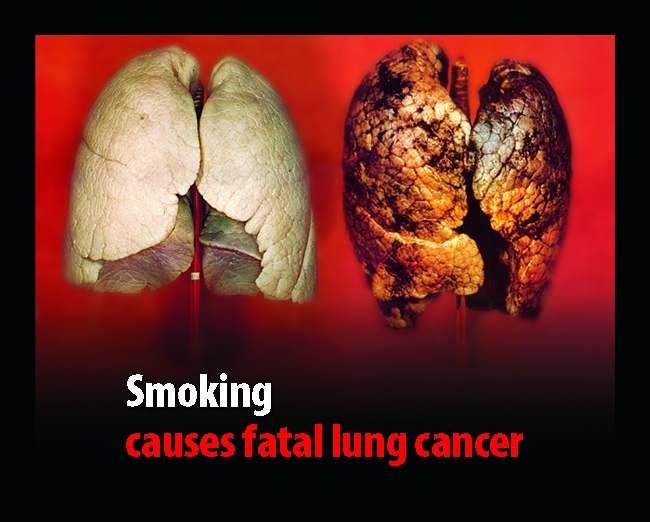
breast cancer. The incidence of lung cancer is strongly correlated with
cigarette smoking, with about 90% of lung cancers arising as a result of
tobacco use.
Lung cancer facts
- Lung cancer is the number one cause of cancer deaths in both men and women in the U.S. and worldwide.
- Cigarette smoking is the principal risk factor for development of lung cancer.
- Passive exposure to tobacco smoke also can cause lung cancer.
- The two types of lung cancer, which grow and spread differently,
are the small cell lung cancers (SCLC) and non-small cell lung cancers
(NSCLC).
- The stage of lung cancer refers to the extent to which the cancer has spread in the body.
- Treatment of lung cancer can involve a combination of surgery, chemotherapy, and radiation therapy as well as newer experimental methods.
- The general prognosis of lung cancer is poor, with overall survival rates of about 16% at 5 years.
- Smoking cessation is the most important measure that can prevent the development of lung cancer.
What is lung cancer?
Cancer of the lung, like all cancers, results from an abnormality in
the body's basic unit of life, the cell. Normally, the body maintains a
system of checks and balances on cell growth so that cells divide to
produce new cells only when new cells are needed. Disruption of this
system of checks and balances on cell growth results in an uncontrolled
division and proliferation of cells that eventually forms a mass known
as a tumor.
Tumors can be benign or malignant; when we speak of "cancer," we are
referring to those tumors that are malignant. Benign tumors usually can
be removed and do not spread to other parts of the body. Malignant
tumors, on the other hand, grow aggressively and invade other tissues of
the body, allowing entry of tumor cells into the bloodstream or
lymphatic system and then to other sites in the body. This process of
spread is termed
metastasis; the areas of tumor growth at these distant sites are called
metastases.
Since lung cancer tends to spread or metastasize very early after it
forms, it is a very life-threatening cancer and one of the most
difficult cancers to treat. While lung cancer can spread to any organ in
the body, certain locations -- particularly the adrenal glands, liver,
brain, and bones -- are the most common sites for lung cancer
metastasis.
The lung also is a very common site for metastasis from tumors in
other parts of the body. Tumor metastases are made up of the same type
of cells as the original (primary) tumor. For example, if prostate
cancer spreads via the bloodstream to the lungs, it is metastatic
prostate cancer in the lung and is not lung cancer.
The principal function of the lungs is to exchange gases between the
air we breathe and the blood. Through the lung, carbon dioxide is
removed from the bloodstream and oxygen from inspired air enters the
bloodstream. The right lung has three lobes, while the left lung is
divided into two lobes and a small structure called the lingula that is
the equivalent of the middle lobe on the right. The major airways
entering the lungs are the bronchi, which arise from the trachea. The
bronchi branch into progressively smaller airways called bronchioles
that end in tiny sacs known as alveoli where gas exchange occurs. The
lungs and chest wall are covered with a thin layer of tissue called the
pleura.